I. Introduction — When the Heart Sends a Warning

Angina is not a heart attack — but it is a cry for help. It is the heart saying, “I’m not getting enough oxygen. Something is wrong.”
For many people, this sensation shows up as tightness, pressure, or discomfort in the chest. For others, it is a burning in the stomach, a heaviness in the jaw, or an unexplained wave of fatigue.
In African, Caribbean, and Black (ACB) communities, heart disease often appears earlier and more aggressively. Understanding angina in these communities can be life-saving. Recognizing these signs is not just medical awareness — it is empowerment, protection, and prevention.
II. A Long Human Story — The History of Angina
Ancient Roots (1500 BCE and Beyond)

Angina has been part of the human story for thousands of years.
- Ancient Egyptian papyrus texts described chest pain. Studies of mummies reveal signs of atherosclerosis, proving heart disease is not just a modern illness.
- In Mesopotamia, healers noted “palpitations.”
- In Vedic Indian medicine, a condition called Hridaya Roga linked heart distress to diet, stress, and physical exertion.
Medieval to Renaissance Breakthroughs
The humoral theory dominated medical thinking, leading to misguided treatments like bloodletting. But change came:
- The Renaissance era brought new anatomical discoveries.
- In 1628, William Harvey transformed medicine by explaining blood circulation.
Formal Naming in the 18th Century
In 1768, Dr. William Heberden formally described “Angina Pectoris,” meaning strangling in the chest.
Shortly after, Edward Jenner linked angina to blocked coronary arteries — a groundbreaking insight.
Modern Advances (19th–20th Century)
The pieces came together:
- In 1809, Allan Burns proposed “myocardial ischemia” as the cause — reduced blood flow to the heart muscle.
- ECG machines, coronary angiography, and imaging breakthroughs reshaped diagnosis.
- Medications like nitroglycerin, beta-blockers, and statins revolutionized care.
- Surgeries such as coronary artery bypass grafting (CABG) saved millions of lives.
Humanity has been wrestling with angina for centuries — but never with tools as powerful as today.
III. Angina Today — How It Shows Up, Why It Happens, and What Helps
Types of Angina

Each form tells a different story:
- Stable Angina: Predictable, triggered by exertion, relieved by rest or medication.
- Unstable Angina: Dangerous, sudden, and a medical emergency.
- Prinzmetal (Variant) Angina: Caused by artery spasms, often occurring at rest.
- Microvascular Angina: Tiny vessel dysfunction — more common in women.
- Refractory Angina: Chronic and resistant to standard treatments.
Why It Happens — Primary Causes
- Coronary Artery Disease (CAD) is the number-one cause. Plaque buildup narrows arteries and limits blood flow.
Other contributors include: - Microvascular disease
- Artery spasms
- Severe anemia
- Heart failure
Symptoms That Should Not Be Ignored
Classic symptoms include:
- Chest pressure
- Tightness
- Burning or squeezing sensations
Pain may radiate to the:
- Arms
- Neck
- Jaw
- Back
- Upper stomach
Atypical symptoms — more common in women, older adults, and people with diabetes — include:
- Nausea
- Dizziness
- Sweating
- Shortness of breath
- Unexplained fatigue
- A sudden sense of dread
How Doctors Diagnose Angina

Diagnosis may include:
- Medical and family history
- Electrocardiogram (ECG)
- Blood tests
- Exercise or pharmacological stress tests
- Echocardiogram
- CT angiography
- Cardiac MRI
- Invasive coronary angiography
A crucial point: a normal ECG does not rule out angina.
Conditions like INOCA (Ischemia with Non-Obstructed Coronary Arteries) require more detailed testing and are often missed.
IV. The Complexities — Debates and Diagnostic Challenges
1. Angina Can Look Like Other Conditions
Symptoms overlap with:
- Acid reflux
- Muscle pain
- Panic attacks
- Lung problems
- Rib injuries
In women, seniors, and people with diabetes, symptoms are often subtle — leading to delays.
2. The Pain Problem
Pain is subjective. Two people can feel angina completely differently. This makes diagnosis more challenging and sometimes frustrating.
3. Controversies in Treatment
The biggest debate today: Do all stable angina patients need stents?
Large trials — ORBITA and ISCHEMIA — showed that optimal medical therapy can be just as effective as stenting. This is true in many stable cases. It can improve symptoms and prevent major events.
This DOES NOT mean stents are unnecessary.
Stents and bypass surgery are life-saving for severe blockages.
But for mild-to-moderate cases, treatment must be personalized.
4. Evolving Guidelines
Medical guidelines continue to evolve as research grows.
The 2024 ESC Guidelines expand recommendations for complex cases like INOCA. They also expand guidelines for microvascular angina. This helps doctors address conditions once overlooked.
V. The Future — Hope on the Horizon

Angina care is entering a new era shaped by innovation, technology, and personalized care.
New Medications & Emerging Therapies
Promising advances include:
- AUX-001 (Nicorandil)
- Improved versions of ranolazine
- Ivabradine and trimetazidine
- Gene therapy aimed at growing new blood vessels
Innovative Procedures
- Personalized stent technology
- Coronary sinus reducers for severe refractory angina
- Laser transmyocardial revascularization (TMR)
Smarter Diagnostics
- High-sensitivity troponin tests
- AI-powered pattern recognition
- Advanced imaging to detect microvascular dysfunction
The Rise of Remote Monitoring
Wearable ECG devices, smartwatches, and telehealth systems now allow:
- Continuous monitoring
- Symptom tracking
- Faster medical intervention
- Better access for rural and underserved communities
The future of angina care is more precise, more personalized, and more accessible than ever before.
VI. Conclusion — Knowledge Is Protection
The story of angina has a long history. It stretches from ancient civilizations to cutting-edge technology. However, one truth remains:
Your heart speaks before it breaks.
Understanding angina includes knowing its symptoms, risks, and treatments. This knowledge is one of the most powerful steps you can take to protect your health.
If you ever feel chest discomfort, unexplained fatigue, breathlessness, or pressure that feels “not normal,” seek medical attention immediately. Your heart deserves to be heard.
And remember:
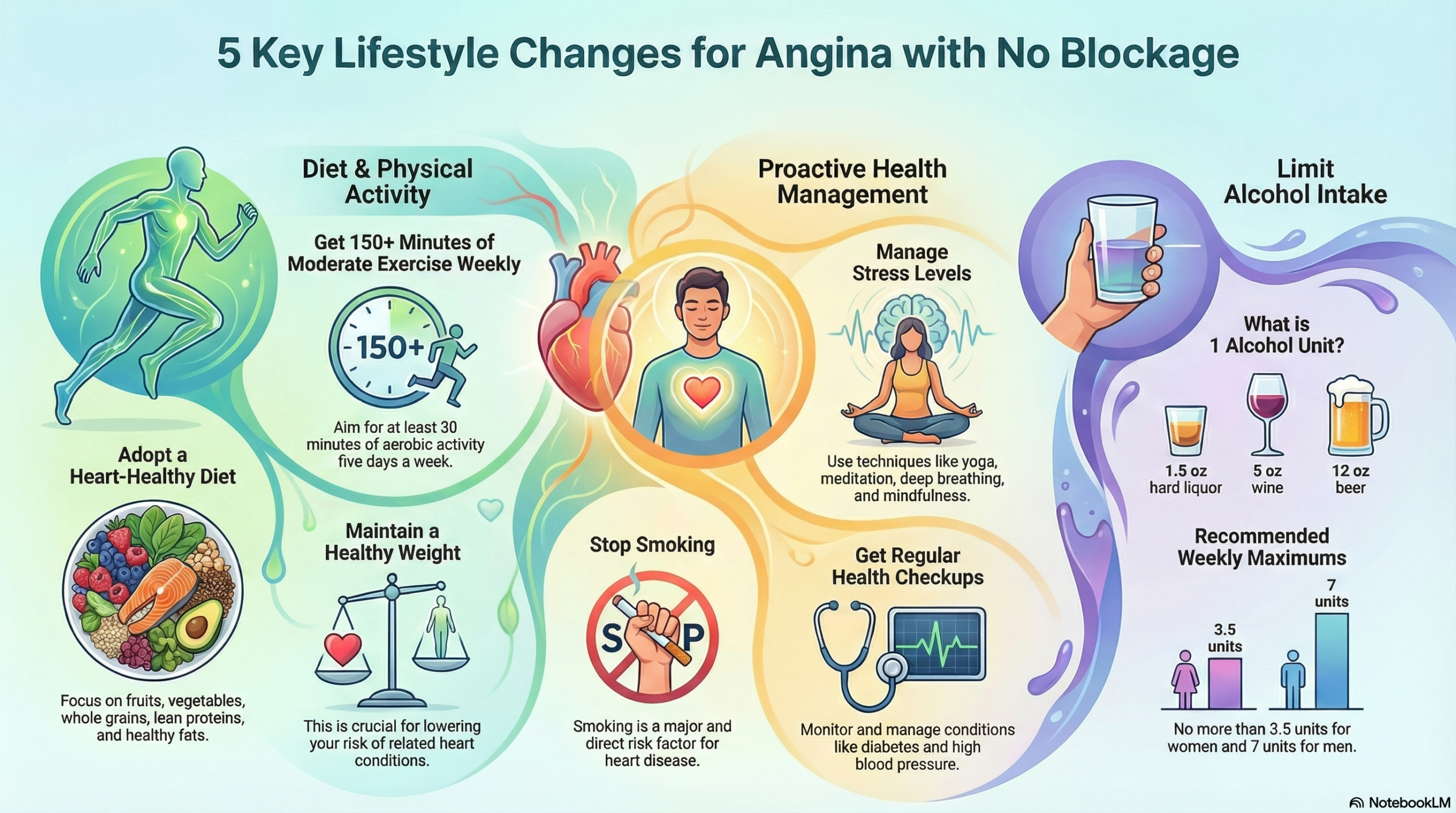
Maintain a heart-healthy lifestyle. Early diagnosis and ongoing care are crucial. They can dramatically reduce the risk of heart attacks, disability, and long-term complications.
Your heart is your story. Protect it. Strengthen it. Listen when it speaks.