Reviewed & Edited by AMHG Editorial Team
Introduction: Beyond the Headlines

During the COVID-19 pandemic, the world saw the letters “ARDS” more than ever before. Many people connected it with the most severe cases of the virus. But that was only the beginning of the story.
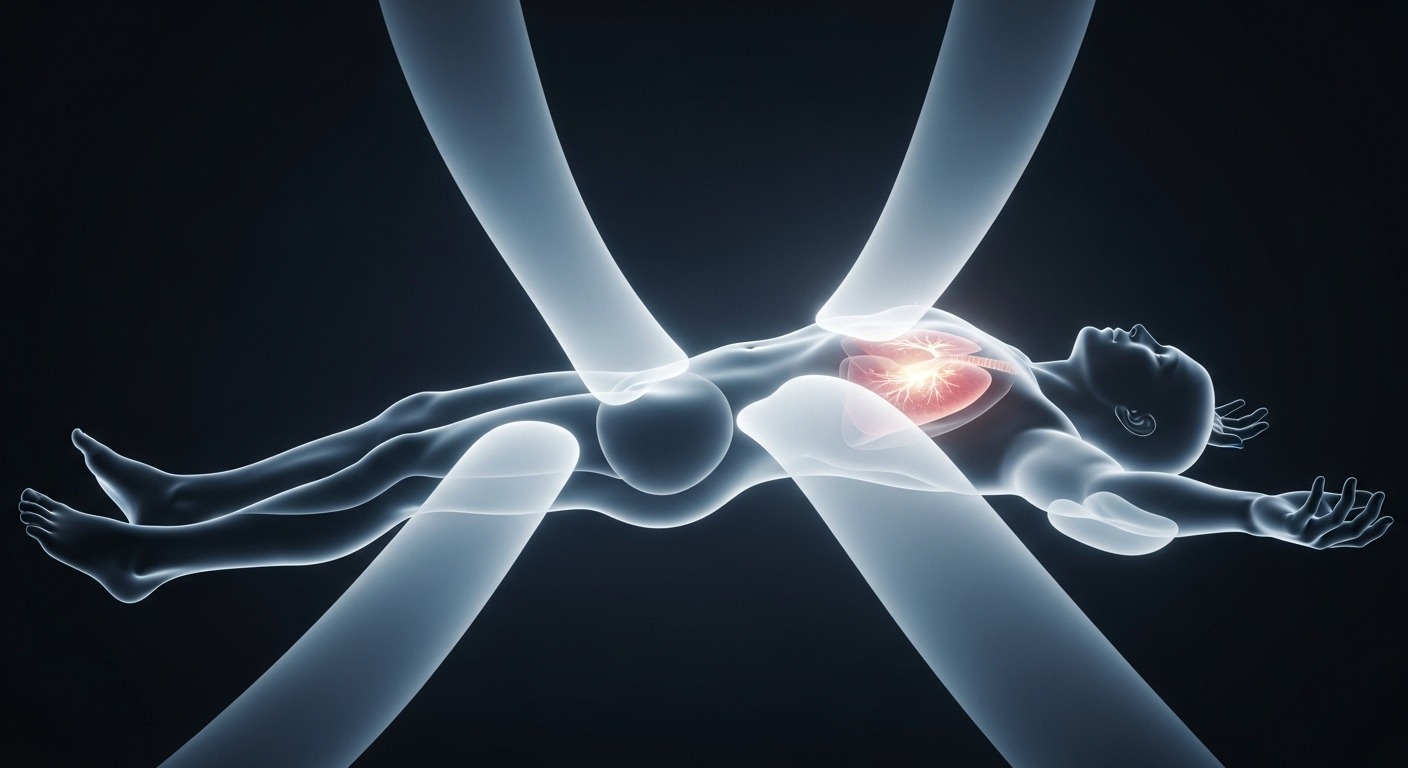
Acute Respiratory Distress Syndrome (ARDS) is far more complex, more dangerous, and more surprising than most people realize. It is not just a lung problem. It is a full-body emergency. This situation exposes how fragile the human body becomes when its systems are pushed to the edge.
In this AMHG investigative report, we go deeper than headlines. We uncover four important truths. These truths reveal how ARDS begins. They show how the body reacts. They also explain how doctors fight it. Finally, they highlight what survivors face long after the crisis ends.
1. The Injury Doesn’t Have to Start in Your Lungs
Most people assume a severe lung condition must begin with damage to the lungs themselves. Sometimes this is true.
Direct lung injuries like:
can trigger ARDS.
But here’s the surprising part: ARDS can begin even when the lungs are not the primary target.
This is called an indirect lung injury, and it can be triggered by events happening in other organs, such as:
- sepsis, a dangerous overreaction to infection
- severe injuries, like major fractures or head trauma
- pancreatitis, an inflamed pancreas
These conditions can cause a chain reaction. Chemicals released during the crisis travel through the bloodstream and damage the lungs from the inside. Suddenly the air sacs fill with fluid, surfactant breaks down, and the lungs begin to fail.
This interconnectedness is striking. Two conditions alone — pneumonia and sepsis — account for 40% to 60% of all ARDS cases. A problem that starts in the abdomen or in a broken bone can end in the lungs.
2. The Body’s Defense System Can Make ARDS Worse

When ARDS begins, the body reacts instantly. The immune system sends cytokines and powerful white blood cells called neutrophils to fight the injury.
In a normal healing process, this response is helpful. But in ARDS, the same defense meant to protect the lungs begins to harm them.
The damaged lung tissue becomes leaky. Immune cells and inflammatory proteins spill into the bloodstream and travel throughout the body. Instead of staying in one place, the inflammation spreads.
This causes:
- more lung damage
- dangerous drops in oxygen
- stress on the heart and other organs
- the risk of multi-organ failure
It is one of the cruelest parts of ARDS: the body’s attempt to heal can become part of the harm.
3. There Is No Cure — Only Support
Many people believe modern medicine has a drug or machine to “fix” almost anything. ARDS is a stark reminder that this is not always true.
There is no direct cure for ARDS.
The treatment does not repair the lungs. Instead, doctors try to keep the person alive long enough for the lungs to heal themselves.
Supportive treatments include:
- oxygen therapy
- mechanical ventilators to take over breathing
- prone positioning (lying the patient on their stomach) to improve oxygen flow
- treating the underlying cause, such as infection or trauma
Dr. Lauren Ferrante, a pulmonary specialist at Yale Medicine, explains:
“We can support the body, but the lungs still have to begin healing on their own. There is no magic bullet.”
This reality makes ARDS one of the most challenging conditions in critical care.
4. For Survivors, the Battle Isn’t Over

Surviving ARDS is a major victory — but recovery can be long and difficult.
Even in top-level ICUs, 25% to 40% of people with ARDS do not survive. Outcomes depend on many factors:
- type of injury
- age
- chronic conditions
- severity of inflammation
- time spent on a ventilator
Those who do survive often face a long road ahead.
Most rebuild lung function within six months to a year, but it requires intense effort.
Survivors often need:
- months of physical therapy
- help regaining muscle strength
- support for memory or concentration problems
- treatment for anxiety, depression, or PTSD
Some never fully regain their lung capacity. For them, simple activities like climbing stairs or carrying groceries may feel harder for the rest of their lives.
ARDS doesn’t only scar the lungs. It can leave emotional scars as well.
Conclusion: A Fragile Balance

ARDS reveals something powerful about the human body. The systems that keep us alive are connected — beautifully and sometimes dangerously. An injury in one organ can create chaos in another. A protective immune response can turn harmful. A life can depend on machines while the lungs slowly repair themselves.
Understanding these truths helps us respect the delicate balance inside our bodies. It also reminds us how quickly that balance can shift.
The next time you hear about ARDS, remember:
It is not just a lung condition.
It is a whole-body emergency.
And survival depends on timing, teamwork, and the incredible resilience of the human body.
Like, share, and subscribe to AMHG Magazine—because knowledge heals, stories inspire, and truth transforms. Every click fuels a movement where culture meets courage, and wellness becomes power. Don’t just watch change—be the heartbeat behind it.