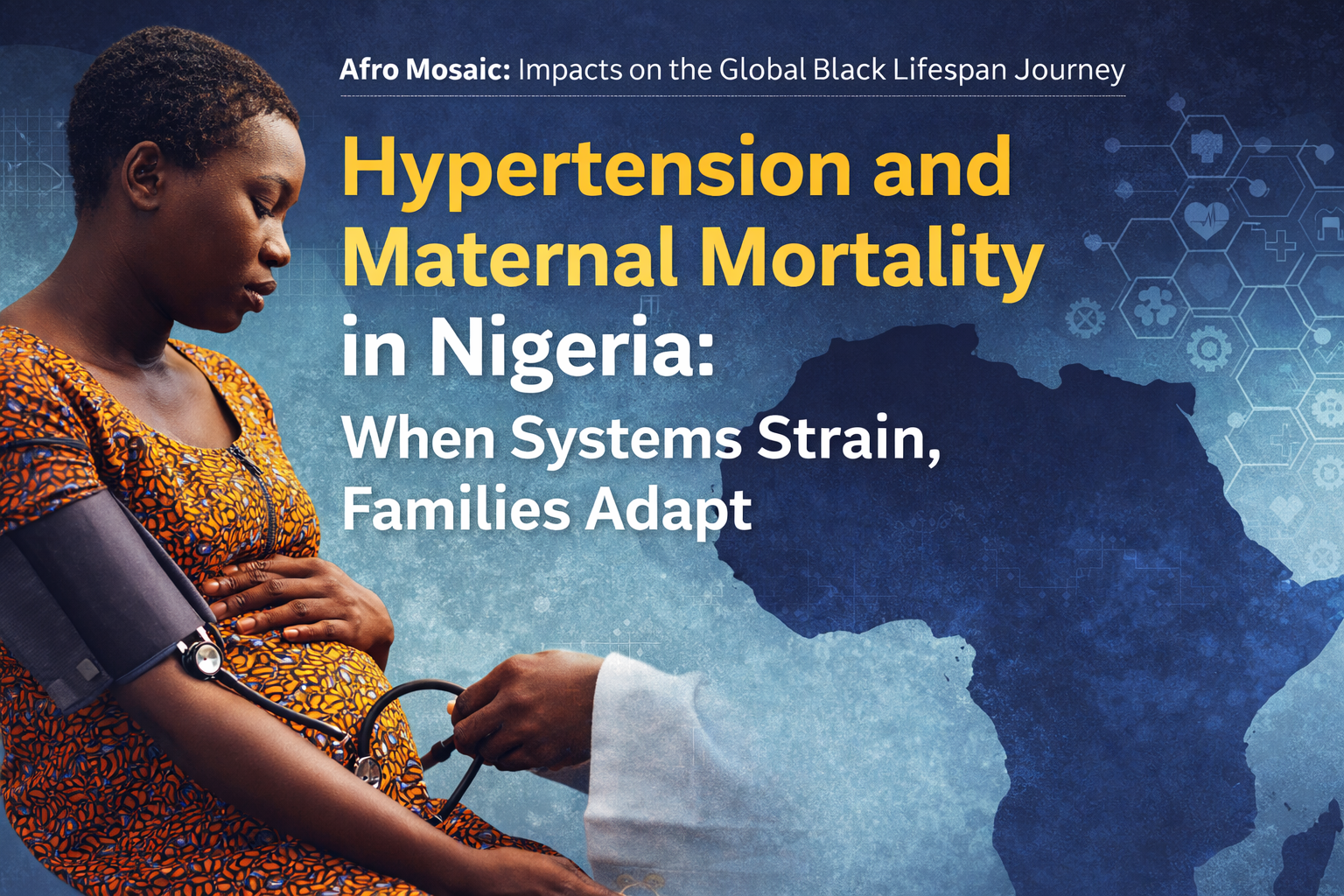
1. The Lifespan Journey: Why Maternal Health is Our Collective Foundation

In our ongoing exploration of the “Afro Mosaic,” we recognize that the health of a nation is not measured by the wealth of its cities, but by the survival of its mothers. Maternal health is the foundational thread of the Global Black Lifespan Journey. When we protect a mother at birth, we are not just saving one life; we are securing the first step of a healthy 100-year lifespan for the next generation.
In Nigeria, however, this foundation is under a state of siege. Our country currently faces a maternal mortality rate of 1,047 deaths per 100,000 live births. This is more than a statistic; it is a systemic betrayal, as Nigeria contributes a staggering 29% of all maternal deaths globally. At the center of this crisis are Hypertensive Disorders of Pregnancy (HDP). We must be clear: HDP is not a “lifestyle failure” or a result of individual negligence. It is a high-risk medical condition that demands a robust, systemic shield of protection—a shield that, far too often, is nowhere to be found.
2. Decoding the Risks: Understanding Hypertensive Disorders of Pregnancy (HDP)

To demand better care, we must first understand the language of the system. HDP is the leading cause of maternal morbidity and mortality in Nigeria. These conditions are defined as follows:
- Chronic Hypertension: High blood pressure that exists before pregnancy or is diagnosed before the 20th week of gestation.
- Gestational Hypertension: New-onset high blood pressure occurring after 20 weeks of pregnancy without protein in the urine.
- Preeclampsia: A multi-system disorder after 20 weeks characterized by high blood pressure and protein in the urine, signaling potential organ damage.
- Eclampsia: A severe, life-threatening complication of preeclampsia involving seizures.
- HELLP Syndrome: The most dangerous variant of preeclampsia. In plain terms, it means the body’s red blood cells are breaking down, the liver is struggling to filter toxins, and the blood is losing its ability to clot. It is a total systemic breakdown.
The danger does not vanish once the baby is born. The “4th Trimester”—the postpartum period—is a treacherous window where 50% of maternal deaths in Sub-Saharan Africa occur. As care transitions from specialists to general clinics, mothers are often left vulnerable to strokes and heart failure.
3. System Strain: Where the Shield of Protection Breaks

Our investigation into the University of Abuja Teaching Hospital (UATH) reveals that maternal deaths from HDP are “potentially preventable with timely and effective care.” Why, then, are they happening? The answer lies in the “System Strain”:
- The Scandal of the “Indigent Patient”: We find a heartbreaking reality where mothers are medically fit for discharge but are held in hospitals because they cannot pay their bills. Financial barriers turn hospitals into debtors’ prisons rather than sanctuaries of healing.
- Inadequate Manpower: Wards are chronically understaffed. Overworked nurses and midwives are stretched so thin they cannot provide the intensive monitoring HDP requires.
- Transportation Deserts: A referral to a tertiary center means nothing if a mother has no reliable way to get there or return for life-saving follow-ups.
- Inconsistent Protocols: A lack of unified management between departments means a mother’s care can depend entirely on which door she walks through.
“Most maternal deaths from HDP are potentially preventable with timely and effective care.”
4. Cultural & Community Resilience: Adaptation as Survival

When the formal system strains to the breaking point, Nigerian families do what they have always done: they adapt. But let us be clear—this resilience is a response to system failure, not a replacement for government responsibility.
- Home Blood Pressure Monitoring (HBPM): Much like managing diabetes with a glucometer, families are adopting HBPM. It is a simple, feasible tool that gives mothers a sense of ownership over their health.
- Task-Shifting: To bridge the gap left by a shortage of doctors, Community Health Extension Workers (CHEWs) and nurses are being trained to initiate care and screen for risks.
- The Mobile Bridge: In a country where nearly everyone has a phone, text messaging and calls are becoming the life-saving bridge over the 4th-trimester gap, ensuring high-risk patients do not “drop out” of care once they return home.
5. The Blueprint for Protection: What Every Family Should Know

The National Guidelines for Prevention and Management of Hypertension in Nigeria (2023-2028) are not just for doctors; they are a bill of rights for every family. To navigate a strained system, you must know the standard you are entitled to.
Core Requirements for Proper Care:
- The Diagnostic Threshold: Hypertension is 140/90 mmHg recorded on two different days. If it hits 180/110 mmHg, it is a crisis that requires immediate diagnosis and intervention.
- The High-Risk Goal: If a mother has diabetes or kidney disease, the system must aim for a target of 130/80 mmHg.
- The Right to Dignity: Every patient has the right to informed consent and a clear clinical evaluation of their condition.
- The Drug Protocol: Families should know the standard “ladder” of care. It often begins with Amlodipine 5mg, moving to a combination with Losartan 50mg, and eventually adding Hydrochlorothiazide (HCTZ) 25mg if targets aren’t met.
The Promise vs. The Reality
| The Promise (National Guidelines) | The Reality (Observed Barriers) |
| Validated electronic or manual equipment for all checks. | Inadequate, broken, or uncalibrated equipment in many wards. |
| Consistent monitoring through the 4th Trimester. | 50% of deaths occur postpartum due to a lack of transition care. |
| Uniform care protocols across all departments. | Inconsistent use of management protocols leading to varied care. |
| Dedicated staff for intensive monitoring. | Overworked nurses and midwives unable to meet the additional workload. |
6. Prevention Through Policy and Action

True protection for the Black lifespan happens before a mother ever enters a labor ward. It requires the exercise of Economic Power and Legal Realities.
- Legal Protections: The government has a “Duty of Care” to provide validated equipment and trained staff. Furthermore, population-based approaches—such as mandatory salt and sugar regulations in processed foods and clear food labeling—are more effective than simply telling a mother to “eat better.”
- Economic Protections: The National Health Insurance Scheme (NHIS) is a critical shield, often covering 90% of costs for those enrolled. We must demand the expansion of this coverage to ensure no mother is held hostage by a hospital bill.
7. Conclusion: Preventable, Not Inevitable
HDP accounts for 32% of maternal deaths in Nigerian referral hospitals. These are not “acts of fate” or “God’s will.” They are the preventable outcomes of a system under strain. By moving from a culture of individual blame to one of systemic accountability, we can close the knowledge-to-action gap.
Protecting the heart of the mother is the only way to protect the 100-year future of our nation. These deaths are preventable with a system designed to honor and protect Black life. Every mother deserves a healthcare shield that is as strong as her own heart.
Why readers should explore this presentation
This presentation offers more than statistics—it explains why hypertension and maternal mortality in Nigeria remain urgent threats to the Black lifespan, and how those outcomes are shaped long before a woman enters a hospital. Grounded in the Afro Mosaic framework, it integrates health, legal protection, social support, and economic power into a coherent narrative. CLICK: https://amhg.ca/wp-content/uploads/2026/02/Nigeria_Hypertension_Maternal_Shield.pdf

CLICK: https://amhg.ca/wp-content/uploads/2026/02/Nigeria_Hypertension_Maternal_Shield.pdf
Readers will gain culturally grounded insight into how system strain—not biology—drives risk, while also seeing the resilience of families, clinicians, and communities navigating gaps in care. Most importantly, it translates complex evidence into practical, protective knowledge that empowers women, families, advocates, and decision-makers.This is essential viewing for anyone who believes maternal survival is a systems issue—and that informed action today protects generations tomorrow.
Why viewers should watch this video: CLICK:https://www.youtube.com/watch?v=cgE9cTRSrJo&feature=youtu.be. This video helps viewers understand why hypertension and maternal mortality in Nigeria are not medical mysteries, but predictable outcomes of system strain. It breaks down how delayed diagnosis, overwhelmed health facilities, financial barriers, and gaps in accountability turn a preventable condition into a life-threatening risk for mothers.
Rather than focusing on individual behavior or culture, the video centers systems—and shows how families are forced to adapt when protection fails. Viewers will come away with clearer insight into how maternal health shapes the entire Black lifespan, why prevention must start long before labor, and what informed, systems-level action actually looks like.
This is essential viewing for anyone interested in maternal health, health equity, and how policy and access determine who survives pregnancy—and who does not.
Why Readers Should Review This Presentation Slide
This presentation slide introduces one of the most critical conversations in maternal health: how hypertension and system strain shape maternal survival in Nigeria. It sets the tone for Series 6 of Impacts on the Global Black Lifespan Journey, grounding the discussion in protection, accountability, and prevention.

https://amhg.ca/wp-content/uploads/2026/02/Nigeria_Hypertension_Maternal_Shield-2.pdf
Readers should review this slide because it clearly frames maternal mortality not as an individual or cultural failure, but as a systems issue that begins long before labor. It connects health, legal realities, social support, and economic access into one unified message: protecting mothers protects the entire Black lifespan.
The slide also reinforces the mission of Afro Mosaic Health Guide Magazine—to transform clinical disparities into protective, actionable knowledge. It prepares viewers to think critically, engage responsibly, and understand why maternal health is foundational to generational survival and dignity.